Excretory System: Functions, Organs, Structure and Facts
Excretory System
The Excretory system is responsible for the elimination of wastes produced by homeostasis.
Humans must get rid of two types of wastes. Wastes from the digestive system (feces) and wastes from metabolic activities (sweat & urine). Removing digestive wastes (pooping) is called egestion. Removing metabolic wastes is called excretion.
Major Metabolic Wastes
The below table summarizes the four types of metabolic wastes produced by humans(and other animals), and the type of chemical reactions that produce them.- Dehydration synthesis = reactions in which small molecules are combined to form large molecules
- Cellular respiration = chemical reaction that releases energy from organic molecules (usually glucose and fatty acids)
- Neutralization = reactions between acids & bases
- Deamination = removal of amino groups from protein molecules.
HUMAN EXCRETORY ORGANS
There are 4 excretory organs in human: The skin, the lungs, the liver, and the kidney(Urinary system).
THE SKIN
The skin excretes the sweat outside the body through numerous pores in the surface of this organ. Sweat is a mixture of three metabolic wastes: water, salts, and urea. So as you sweat, your body accomplishes two things: 1) sweating has a cooling effect on the body, and 2) metabolic wastes are excreted.The skin is formed of two layers; the thin epidermis at the top, and the thicker dermis below. The inner layer of skin (dermis) contains the oil glands, hair follicles, fatty layers, nerves, and sweat glands. The sweat gland leads to the sweat duct (tube) which opens on the skin surface through a pore.
Sweat formation
Notice that the sweat gland is a tubular structure tangled with the blood capillaries. This close association of tubes allows wastes (namely water, salts, and urea) to diffuse from the blood into the sweat gland. When body temperature rises, the fluid (sweat) is released from the gland, travels through the duct, and reaches the skin surface through openings called pores.THE LUNGS
Cellular respiration occurs in every living cell in your body. It is the reaction that provides energy (in the form of ATP molecules) for cellular activities. If respiration stops, the cell no longer has energy for cellular activities, and the cell dies.As respiration occurs carbon dioxide is produced as a waste product. As the carbon dioxide accumulates in body cells, it eventually diffuses out of the cells and into the bloodstream, which eventually circulates to the lungs. In the alveoli of the lungs, carbon dioxide diffuses from the blood, into the lung tissue, and then leaves the body every time we exhale. Some water vapor also exits the body during exhalation.
THE LIVER
The liver is a large, important organ in our bodies. Its numerous functions make it "part" of the circulatory, digestive, and excretory systems.Liver as an excretory organ acts to breakdown some proteins and other nitrogenous compounds by a process called deamination. As a result of these reactions, a nitrogenous waste called urea is formed. Liver as well as helps in excreting toxic substances, drugs, and their derivatives; and bile pigments and cholesterol.
THE URINARY SYSTEM IN HUMAN
(THE KIDNEY)
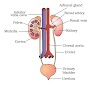
In humans, the excretory system consists of a pair of kidneys, one pair of ureters, a urinary bladder and a urethra. Kidneys are reddish brown, bean shaped structures situated between the levels of last thoracic and third lumbar vertebra close to the dorsal inner wall of the abdominal cavity.
Generally, excretion means the separation and elimination of waste materials
from the body through a special structure called the excretory organ. Specifically, the act of excretion is a two-fold function: it eliminates substances that have reached their threshold concentration in the blood, and it retains or reabsorbs substances that are below this concentration. Both functions, however, are homeostatic, tending to maintain a stable environment within the body.
The major functions of the excretory system(kidney) can be summarizes as follows:
- Maintenance of proper concentrations of individual ions (Na+, K+, Cl-, H+, etc.).
- Maintenance of proper body volume by regulating water content.
- Maintenance of osmotic concentrations, which result from the ability of the excretoryy systems to control water and electrolytes contents in the body.
- Removal of metabolic end products (e.g., urea, uric acid, etc.).
- Removal of foreign substances and/or their metabolic products.
EXTERNAL STRUCTURE OF KIDNEY
Two Kidneys
They are dark, red, bean-shaped and lie in the upper part of the abdominal cavity against the dorsal body wall. They are embedded in a protective layer of fat and connective tissue. The right kidney is slightly on a lower level than the left. Each Kidney is about 4½ inches long, 2½ inches broad, and over one inch thick. The weight of each kidney in adult human is about 150 g, so they represent about 0.5% of the total weight of the body.
Two Ureters
They are two slender muscular tubes which take their origin at the hilum of each kidney (from the renal pelvis) and run down to join the urinary bladder.
The Urinary Bladder
The bladder has an elastic wall and placed in the lower part of the abdominal cavity. It supplied with a sphincter muscles at its connection with both the ureters and urethra.
The Urethra
It is a muscular tube which carried the urine from the bladder to the outside.
Renal Vein and Artery
Each kidney receive a renal artery from the aorta, which brings the blood into the kidney. From each kidney, a renal vein is extended to the inferior vena cava, which carries the blood back to the heart.
INTERNAL STRUCTURE OF KIDNEY
Examination of vertical section of the kidney shows that the kidney is made up of:
An Outer Cortex
It made of a dark red tissue, due to the presence of all glomeruli which contain tufts of blood capillaries. The cortex contains all the proximal tubules and distal tubules, and cortical collecting ducts.
An Inner Medulla
It is made of lighter tissue, due to its relative low blood supply. Medulla has a
radial appearance due to the presence of loops of Henle, the vasa recta, and medullary collecting tubules. It is subdivided into:
(i) An outer medulla, which lies next to the cortex and
(ii) An inner medulla which extends out into the renal sinus forming renal papillae. Medulla is differentiated to form a number of cone-like structure known as renal pyramids (10-15) with their apical ends projecting as renal papillae into the calyces of the pelvis.
The Pelvis
It is a funnel-shaped structure which has at its free end number of cup-like cavities called calyces (sing. calyx). The pelvis leads to the ureter.
FUNCTIONS OF KIDNEYS
Excretion of waste products:
Kidneys excrete the waste products which contains nitrogen and sulphur, as well as ketone bodies. They aid in excretion of the drugs, toxic substances, and their derivatives, e.g. penicillin.
Maintenance of constant volume and composition of inside the body:
The kidneys maintain constant volume of body fluids, osmotic pressure, and blood pressure, hence they protect the body from diseases, by excreting excess water and electrolytes. For instances, (i) excess intake of sodium salts (NaCl) leads to hypernatermia accompanied with increased water retention which lead to increase in blood pressure and osmotic pressure, as well as development of oedema. As kidneys capable of to remove the excess NaCl, they prevent the mentioned syndromes. (ii) excess intake of potassium (K+) produces
hyperkalemia which leads to weakness of muscles and this causes troubles in the heart and abdominal muscles. Kidneys remove the excess K+ and keep normal muscle function, e.g. heart beats.
Regulation of arterial blood pressure (ABP):
In case of hypoxia due to hypotension, the kidneys secrete the enzyme renin, via the juxtaglomerular tissue, which converts plasma angiotensigogen to angiotensin I that converted by convertase into angiotensin II.
Angiotensin II acts as (i) a vasoconstrictor leading to raising the blood pressure and (ii) a stimulator for the secretion of both aldosterone from the adrenal cortex and antidiuretic hormone from the posterior pituitary, which cause Na+ and water retention
hereby increasing blood volume and then restoring the blood pressure. The kidneys synthesize a number of prostaglandins (PGs), a vasoactive substances, that act to increase the ABP. PGE2 acts as a vasodilator which can modulate the vasoconstriction induced by sympathetic stimulation.
Regulation of blood pH through preserving acid-base balance In case of acidosis, they secrete H+ and react it with ammonia (NH3) forming ammonium (NH4), which excreted as NH4 salts in the urine. While, in case of alkalosis, the kidneys decrease the secretion of H+, synthesis of NH4, and
reabsorption of bicarbonate (HCO3-); and they increases reabsorption of Cl-.
Enzyme formation:
The kidneys synthesize enzymes such as histaminase to destroy the histamine, phosphatase to remove inorganic phosphate from organic compounds, and cholinesterase to destroy acetylcholine.
Endocrine function:
They regulate the conversion of vitamin D to 1,25 dihyroxycholecalciferol (and also 24,25 dihyroxcholecalciferol) which facilitate the intestinal absorption of calcium and phosphate. It also acts on bone by mobilizing the calcium ion. PTH is required for renal synthesis of 1,25 dihyroxcholecalciferol.
Detoxification:
In the kidney, the toxic substance is converted to a non-toxic compound. For example, the kidneys convert benzoic acid to the hippuric acid by combination with glycine and excrete it through urine to outside. This process occurs mainly in the liver.
THE NEPHRON
The substance of the kidney is made up of a number of structural and functional units called nephrons. Each human kidney contains one million nephrons or more. The nephrons are concerned with the separation of urine from the blood.
It should be noted that there are 2 basic types of nephrons:
Cortical nephrons:
They represent 85% of the nephrons in the kidney. Except for a small portion of the loop of Henle, they're entirely located within the renal cortex. They will play a large role in making sure the blood has the correct ionic and chemical make-up.
Juxtamedullary nephrons:
Their renal corpuscles are located very close to the cortex-medulla junction. Their loops of Henle extend deep into the medulla and can be quite long. They play an important role in the body's ability to concentrate urine, i.e. they are very involved in water reabsorption.
Each nephron has two parts – the glomerulus and the renal tubule.
Glomerulus is a tuft of capillaries formed by the afferent arteriole – a fine branch of renal artery. Blood from the glomerulus is carried away by an efferent arteriole.
The renal tubule begins with a double walled cup-like structure called Bowman’s capsule, which encloses the glomerulus.
Glomerulus alongwith Bowman’s capsule, is called the malpighian body or renal of Kidney corpuscle. The tubule continues further to form a highly coiled network – proximal convoluted tubule.

A hairpin shaped Henle’s loop is the next part of the tubule which has a descending and an ascending limb. The ascending limb continues as another highly coiled tubular region called distal convoluted tubule (DCT). The DCTs of many nephrons open into a straight tube called collecting duct, many of which converge and open into the renal pelvis through medullary pyramids in the calyces.
The Malpighian corpuscle, PCT and DCT of the nephron are situated in the cortical region of the kidney whereas the loop of Henle dips into the medulla. In majority of nephrons, the loop of Henle is too short and extends only very little into the medulla. Such nephrons are called cortical nephrons. In some of the nephrons, the loop of Henle is very long and runs deep into the medulla.
URINE FORMATION
Urine formation involves three main processes namely, glomerular filtration, reabsorption and secretion, that takes place in different parts of the nephron.
The first step in urine formation is the filtration of blood, which is carried out by the glomerulus and is called glomerular filtration. On an average, 1100-1200 ml of blood is filtered by the kidneys per minute which constitute roughly 1/5th of the blood pumped out by each ventricle of the heart in a minute. The glomerular capillary blood pressure causes filtration of blood through 3 layers, i.e., the endothelium of glomerular blood vessels, the epithelium of Bowman’s capsule and a basement membrane between these two layers. The epithelial cells of Bowman’s capsule called podocytes are arranged in an intricate manner so as to leave some minute spaces called filtration slits or slit pores. Blood is filtered so finely through these membranes, that almost all the constituents of the plasma except the proteins pass onto the lumen of the Bowman’s capsule. Therefore, it is considered as a process of ultra filtration.The amount of the filtrate formed by the kidneys per minute is called glomerular filtration rate (GFR). GFR in a healthy individual is approximately 125 ml/minute, i.e., 180 litres per day !
The kidneys have built-in mechanisms for the regulation of glomerular filtration rate. One such efficient mechanism is carried out by juxta glomerular apparatus (JGA). JGA is a special sensitive region formed by cellular modifications in the distal convoluted tubule and the afferent arteriole at the location of their contact. A fall in GFR can activate the JG cells to release renin which can stimulate the glomerular blood flow and thereby the GFR back to normal.
A comparison of the volume of the filtrate formed per day (180 litres per day) with that of the urine released (1.5 litres), suggest that nearly 99 per cent of the filtrate has to be reabsorbed by the renal tubules. This process is called reabsorption. The tubular epithelial cells in different segments of nephron perform this either by active or passive mechanisms. For example, substances like glucose, amino acids, Na+, etc., in the filtrate are reabsorbed actively whereas the nitrogenous wastes are absorbed by passive transport. Reabsorption of water also occurs passively in the initial segments of the nephron.During urine formation, the tubular cells secrete substances like H+,K+ and ammonia into the filtrate. Tubular secretion is also an important step in urine formation as it helps in the maintenance of ionic and acid base balance of body fluids.
REGULATION OF KIDNEY FUNCTION
The functioning of the kidneys is efficiently monitored and regulated by hormonal feedback mechanisms involving the hypothalamus, JGA and to a certain extent, the heart.
Osmoreceptors in the body are activated by changes in blood volume, body fluid volume and ionic concentration. An excessive loss of fluid from the body can activate these receptors which stimulate the hypothalamus to release antidiuretic hormone (ADH) or vasopressin from the neurohypophysis. ADH facilitates water reabsorption from latter parts of the tubule, thereby preventing diuresis. An increase in body fluid volume can switch off the osmoreceptors and suppress the ADH release to complete the feedback. ADH can also affect the kidney function by its constrictory effects on blood vessels. This causes an increase in blood pressure. An increase in blood pressure can increase the glomerular blood flow and thereby the GFR.
The JGA plays a complex regulatory role. A fall in glomerular blood flow/glomerular blood pressure/GFR can activate the JG cells to release renin which converts angiotensinogen in blood to angiotensin I and further to angiotensin II. Angiotensin II, being a powerful vasoconstrictor, increases the glomerular blood pressure and thereby GFR. Angiotensin II also activates the adrenal cortex to release Aldosterone. Aldosterone causes reabsorption of Na+ and water from the distal parts of the tubule. This also leads to an increase in blood pressure and GFR. This complex mechanism is generally known as the Renin-Angiotensin mechanism.
An increase in blood flow to the atria of the heart can cause the release of Atrial Natriuretic Factor (ANF). ANF can cause vasodilation (dilation of blood vessels) and thereby decrease the blood pressure. ANF mechanism, therefore, acts as a check on the renin-angiotensin mechanism.
MICTURITION
Urine formed by the nephrons is ultimately carried to the urinary bladder where it is stored till a voluntary signal is given by the central nervous system (CNS). This signal is initiated by the stretching of the urinary bladder as it gets filled with urine. In response, the stretch receptors on the walls of the bladder send signals to the CNS. The CNS passes on motor messages to initiate the contraction of smooth muscles of the bladder and simultaneous relaxation of the urethral sphincter causing the release of urine. The process of release of urine is called micturition and the neural mechanisms causing it is called the micturition reflex.
An adult human excretes, on an average, 1 to 1.5 litres of urine per day. The urine formed is a light yellow coloured watery fluid which is slightly acidic (pH-6.0) and has a characterestic odour. On an average, 25-30 gm of urea is excreted out per day. Various conditions can affect the characteristics of urine. Analysis of urine helps in clinical diagnosis of many metabolic discorders as well as malfunctioning of the kidney. For example, presence of glucose (Glycosuria) and ketone bodies (Ketonuria) in urine are indicative of diabetes mellitus.
DISORDERS OF THE EXCRETORY SYSTEM
Malfunctioning of kidneys can lead to accumulation of urea in blood, a condition called uremia, which is highly harmful and may lead to kidney failure. In such patients, urea can be removed by a process called hemodialysis. Blood drained from a convenient artery is pumped into a dialysing unit after adding an anticoagulant like heparin. The unit contains a coiled cellophane tube surrounded by a fluid (dialysing fluid) having the same composition as that of plasma except the nitrogenous wastes. The porous cellophane membrance of the tube allows the passage of molecules based on concentration gradient. As nitrogenous wastes are absent in the dialysing fluid, these substances freely move out, thereby clearing the blood. The cleared blood is pumped back to the body through a vein after adding anti-heparin to it. This method is a boon for thousands of uremic patients all over the world.Kidney transplantation is the ultimate method in the correction of acute renal failures (kidney failure). A functioning kidney is used in transplantation from a donor, preferably a close relative, to minimise its chances of rejection by the immune system of the host. Modern clinical procedures have increased the success rate of such a complicated technique.
Renal calculi: Stone or insoluble mass of crystallised salts (oxalates, etc.) formed within the kidney.
Glomerulonephritis: Inflammation of glomeruli of kidney.
SUMMARY
Many nitrogen containing substances, ions, CO2, water, etc., that accumulate in the body have to be eliminated. Nature of nitrogenous wastes formed and their excretion vary among animals, mainly depending on the habitat (availability of water). Ammonia, urea and uric acid are the major nitrogenous wastes excreted.
Protonephridia, nephridia, malpighian tubules, green glands and the kidneys are the common excretory organs in animals. They not only eliminate nitrogenous wastes but also help in the maintenance of ionic and acid-base balance of body fluids.
In humans, the excretory system consists of one pair of kidneys, a pair of ureters, a urinary bladder and a urethra. Each kidney has over a million tubular structures called nephrons. Nephron is the functional unit of kidney and has two portions – glomerulus and renal tubule. Glomerulus is a tuft of capillaries formed from afferent arterioles, fine branches of renal artery. The renal tubule starts with a double walled Bowman’s capsule and is further differentiated into a proximal convoluted tubule (PCT), Henle’s loop (HL) and distal convoluted tubule (DCT). The DCTs of many nephrons join to a common collecting duct many of which ultimately open into the renal pelvis through the medullary pyramids. The Bowman’s capsule encloses the glomerulus to form Malpighian or renal corpuscle.
Urine formation involves three main processes, i.e., filtration, reabsorption and secretion. Filtration is a non-selective process performed by the glomerulus using the glomerular capillary blood pressure. About 1200 ml of blood is filtered by the glomerulus per minute to form 125 ml of filtrate in the Bowman’s capsule per minute (GFR). JGA, a specialised portion of the nephrons, plays a significant role in the regulation of GFR. Nearly 99 per cent reabsorption of the filtrate takes place through different parts of the nephrons. PCT is the major site of reabsorption and selective secretion. HL primarily helps to maintain osmolar gradient (300 mOsmolL–1 -1200 mOsmolL–1) within the kidney interstitium. DCT and collecting duct allow extensive reabsorption of water and certain electrolytes, which help in osmoregulation: H+, K+ and NH3 could be secreted into the filtrate by the tubules to maintain the ionic balance and pH of body fluids.
A counter current mechanism operates between the two limbs of the loop of Henle and those of vasa recta (capillary parallel to Henle’s loop). The filtrate gets concentrated as it moves down the descending limb but is diluted by the ascending limb. Electrolytes and urea are retained in the interstitium by this arrangement. DCT and collecting duct concentrate the filtrate about four times, i.e., from 300 mOsmolL–1 to 1200 mOsmolL–1, an excellent mechanism of conservation of water. Urine is stored in the urinary bladder till a voluntary signal from CNS carries out its release through urethra, i.e., micturition. Skin, lungs and liver also assist in excretion.
In humans, the excretory system consists of a pair of kidneys, one pair of ureters, a urinary bladder and a urethra. Kidneys are reddish brown, bean shaped structures situated between the levels of last thoracic and third lumbar vertebra close to the dorsal inner wall of the abdominal cavity.
Generally, excretion means the separation and elimination of waste materials
from the body through a special structure called the excretory organ. Specifically, the act of excretion is a two-fold function: it eliminates substances that have reached their threshold concentration in the blood, and it retains or reabsorbs substances that are below this concentration. Both functions, however, are homeostatic, tending to maintain a stable environment within the body.
The major functions of the excretory system(kidney) can be summarizes as follows:
- Maintenance of proper concentrations of individual ions (Na+, K+, Cl-, H+, etc.).
- Maintenance of proper body volume by regulating water content.
- Maintenance of osmotic concentrations, which result from the ability of the excretoryy systems to control water and electrolytes contents in the body.
- Removal of metabolic end products (e.g., urea, uric acid, etc.).
- Removal of foreign substances and/or their metabolic products.
EXTERNAL STRUCTURE OF KIDNEY
Two Kidneys
They are dark, red, bean-shaped and lie in the upper part of the abdominal cavity against the dorsal body wall. They are embedded in a protective layer of fat and connective tissue. The right kidney is slightly on a lower level than the left. Each Kidney is about 4½ inches long, 2½ inches broad, and over one inch thick. The weight of each kidney in adult human is about 150 g, so they represent about 0.5% of the total weight of the body.Two Ureters
They are two slender muscular tubes which take their origin at the hilum of each kidney (from the renal pelvis) and run down to join the urinary bladder.The Urinary Bladder
The bladder has an elastic wall and placed in the lower part of the abdominal cavity. It supplied with a sphincter muscles at its connection with both the ureters and urethra.The Urethra
It is a muscular tube which carried the urine from the bladder to the outside.Renal Vein and Artery
Each kidney receive a renal artery from the aorta, which brings the blood into the kidney. From each kidney, a renal vein is extended to the inferior vena cava, which carries the blood back to the heart.INTERNAL STRUCTURE OF KIDNEY
Examination of vertical section of the kidney shows that the kidney is made up of:An Outer Cortex
It made of a dark red tissue, due to the presence of all glomeruli which contain tufts of blood capillaries. The cortex contains all the proximal tubules and distal tubules, and cortical collecting ducts.An Inner Medulla
It is made of lighter tissue, due to its relative low blood supply. Medulla has aradial appearance due to the presence of loops of Henle, the vasa recta, and medullary collecting tubules. It is subdivided into:
(i) An outer medulla, which lies next to the cortex and
(ii) An inner medulla which extends out into the renal sinus forming renal papillae. Medulla is differentiated to form a number of cone-like structure known as renal pyramids (10-15) with their apical ends projecting as renal papillae into the calyces of the pelvis.
The Pelvis
It is a funnel-shaped structure which has at its free end number of cup-like cavities called calyces (sing. calyx). The pelvis leads to the ureter.FUNCTIONS OF KIDNEYS
Excretion of waste products:
Kidneys excrete the waste products which contains nitrogen and sulphur, as well as ketone bodies. They aid in excretion of the drugs, toxic substances, and their derivatives, e.g. penicillin.Maintenance of constant volume and composition of inside the body:
The kidneys maintain constant volume of body fluids, osmotic pressure, and blood pressure, hence they protect the body from diseases, by excreting excess water and electrolytes. For instances, (i) excess intake of sodium salts (NaCl) leads to hypernatermia accompanied with increased water retention which lead to increase in blood pressure and osmotic pressure, as well as development of oedema. As kidneys capable of to remove the excess NaCl, they prevent the mentioned syndromes. (ii) excess intake of potassium (K+) produceshyperkalemia which leads to weakness of muscles and this causes troubles in the heart and abdominal muscles. Kidneys remove the excess K+ and keep normal muscle function, e.g. heart beats.
Regulation of arterial blood pressure (ABP):
In case of hypoxia due to hypotension, the kidneys secrete the enzyme renin, via the juxtaglomerular tissue, which converts plasma angiotensigogen to angiotensin I that converted by convertase into angiotensin II.
Angiotensin II acts as (i) a vasoconstrictor leading to raising the blood pressure and (ii) a stimulator for the secretion of both aldosterone from the adrenal cortex and antidiuretic hormone from the posterior pituitary, which cause Na+ and water retention
hereby increasing blood volume and then restoring the blood pressure. The kidneys synthesize a number of prostaglandins (PGs), a vasoactive substances, that act to increase the ABP. PGE2 acts as a vasodilator which can modulate the vasoconstriction induced by sympathetic stimulation.
hereby increasing blood volume and then restoring the blood pressure. The kidneys synthesize a number of prostaglandins (PGs), a vasoactive substances, that act to increase the ABP. PGE2 acts as a vasodilator which can modulate the vasoconstriction induced by sympathetic stimulation.
Regulation of blood pH through preserving acid-base balance In case of acidosis, they secrete H+ and react it with ammonia (NH3) forming ammonium (NH4), which excreted as NH4 salts in the urine. While, in case of alkalosis, the kidneys decrease the secretion of H+, synthesis of NH4, and
reabsorption of bicarbonate (HCO3-); and they increases reabsorption of Cl-.
reabsorption of bicarbonate (HCO3-); and they increases reabsorption of Cl-.
Enzyme formation:
The kidneys synthesize enzymes such as histaminase to destroy the histamine, phosphatase to remove inorganic phosphate from organic compounds, and cholinesterase to destroy acetylcholine.Endocrine function:
They regulate the conversion of vitamin D to 1,25 dihyroxycholecalciferol (and also 24,25 dihyroxcholecalciferol) which facilitate the intestinal absorption of calcium and phosphate. It also acts on bone by mobilizing the calcium ion. PTH is required for renal synthesis of 1,25 dihyroxcholecalciferol.Detoxification:
In the kidney, the toxic substance is converted to a non-toxic compound. For example, the kidneys convert benzoic acid to the hippuric acid by combination with glycine and excrete it through urine to outside. This process occurs mainly in the liver.
THE NEPHRON
The substance of the kidney is made up of a number of structural and functional units called nephrons. Each human kidney contains one million nephrons or more. The nephrons are concerned with the separation of urine from the blood.It should be noted that there are 2 basic types of nephrons:
Cortical nephrons:
They represent 85% of the nephrons in the kidney. Except for a small portion of the loop of Henle, they're entirely located within the renal cortex. They will play a large role in making sure the blood has the correct ionic and chemical make-up.
Juxtamedullary nephrons:
Their renal corpuscles are located very close to the cortex-medulla junction. Their loops of Henle extend deep into the medulla and can be quite long. They play an important role in the body's ability to concentrate urine, i.e. they are very involved in water reabsorption.
Each nephron has two parts – the glomerulus and the renal tubule.
Glomerulus is a tuft of capillaries formed by the afferent arteriole – a fine branch of renal artery. Blood from the glomerulus is carried away by an efferent arteriole.
The renal tubule begins with a double walled cup-like structure called Bowman’s capsule, which encloses the glomerulus.
Glomerulus alongwith Bowman’s capsule, is called the malpighian body or renal of Kidney corpuscle. The tubule continues further to form a highly coiled network – proximal convoluted tubule.
 |
A hairpin shaped Henle’s loop is the next part of the tubule which has a descending and an ascending limb. The ascending limb continues as another highly coiled tubular region called distal convoluted tubule (DCT). The DCTs of many nephrons open into a straight tube called collecting duct, many of which converge and open into the renal pelvis through medullary pyramids in the calyces.
The Malpighian corpuscle, PCT and DCT of the nephron are situated in the cortical region of the kidney whereas the loop of Henle dips into the medulla. In majority of nephrons, the loop of Henle is too short and extends only very little into the medulla. Such nephrons are called cortical nephrons. In some of the nephrons, the loop of Henle is very long and runs deep into the medulla.
URINE FORMATION
Urine formation involves three main processes namely, glomerular filtration, reabsorption and secretion, that takes place in different parts of the nephron.
The first step in urine formation is the filtration of blood, which is carried out by the glomerulus and is called glomerular filtration. On an average, 1100-1200 ml of blood is filtered by the kidneys per minute which constitute roughly 1/5th of the blood pumped out by each ventricle of the heart in a minute. The glomerular capillary blood pressure causes filtration of blood through 3 layers, i.e., the endothelium of glomerular blood vessels, the epithelium of Bowman’s capsule and a basement membrane between these two layers. The epithelial cells of Bowman’s capsule called podocytes are arranged in an intricate manner so as to leave some minute spaces called filtration slits or slit pores. Blood is filtered so finely through these membranes, that almost all the constituents of the plasma except the proteins pass onto the lumen of the Bowman’s capsule. Therefore, it is considered as a process of ultra filtration.The amount of the filtrate formed by the kidneys per minute is called glomerular filtration rate (GFR). GFR in a healthy individual is approximately 125 ml/minute, i.e., 180 litres per day !
The kidneys have built-in mechanisms for the regulation of glomerular filtration rate. One such efficient mechanism is carried out by juxta glomerular apparatus (JGA). JGA is a special sensitive region formed by cellular modifications in the distal convoluted tubule and the afferent arteriole at the location of their contact. A fall in GFR can activate the JG cells to release renin which can stimulate the glomerular blood flow and thereby the GFR back to normal.
A comparison of the volume of the filtrate formed per day (180 litres per day) with that of the urine released (1.5 litres), suggest that nearly 99 per cent of the filtrate has to be reabsorbed by the renal tubules. This process is called reabsorption. The tubular epithelial cells in different segments of nephron perform this either by active or passive mechanisms. For example, substances like glucose, amino acids, Na+, etc., in the filtrate are reabsorbed actively whereas the nitrogenous wastes are absorbed by passive transport. Reabsorption of water also occurs passively in the initial segments of the nephron.During urine formation, the tubular cells secrete substances like H+,K+ and ammonia into the filtrate. Tubular secretion is also an important step in urine formation as it helps in the maintenance of ionic and acid base balance of body fluids.
REGULATION OF KIDNEY FUNCTION
The functioning of the kidneys is efficiently monitored and regulated by hormonal feedback mechanisms involving the hypothalamus, JGA and to a certain extent, the heart.
Osmoreceptors in the body are activated by changes in blood volume, body fluid volume and ionic concentration. An excessive loss of fluid from the body can activate these receptors which stimulate the hypothalamus to release antidiuretic hormone (ADH) or vasopressin from the neurohypophysis. ADH facilitates water reabsorption from latter parts of the tubule, thereby preventing diuresis. An increase in body fluid volume can switch off the osmoreceptors and suppress the ADH release to complete the feedback. ADH can also affect the kidney function by its constrictory effects on blood vessels. This causes an increase in blood pressure. An increase in blood pressure can increase the glomerular blood flow and thereby the GFR.
The JGA plays a complex regulatory role. A fall in glomerular blood flow/glomerular blood pressure/GFR can activate the JG cells to release renin which converts angiotensinogen in blood to angiotensin I and further to angiotensin II. Angiotensin II, being a powerful vasoconstrictor, increases the glomerular blood pressure and thereby GFR. Angiotensin II also activates the adrenal cortex to release Aldosterone. Aldosterone causes reabsorption of Na+ and water from the distal parts of the tubule. This also leads to an increase in blood pressure and GFR. This complex mechanism is generally known as the Renin-Angiotensin mechanism.
An increase in blood flow to the atria of the heart can cause the release of Atrial Natriuretic Factor (ANF). ANF can cause vasodilation (dilation of blood vessels) and thereby decrease the blood pressure. ANF mechanism, therefore, acts as a check on the renin-angiotensin mechanism.
MICTURITION
Urine formed by the nephrons is ultimately carried to the urinary bladder where it is stored till a voluntary signal is given by the central nervous system (CNS). This signal is initiated by the stretching of the urinary bladder as it gets filled with urine. In response, the stretch receptors on the walls of the bladder send signals to the CNS. The CNS passes on motor messages to initiate the contraction of smooth muscles of the bladder and simultaneous relaxation of the urethral sphincter causing the release of urine. The process of release of urine is called micturition and the neural mechanisms causing it is called the micturition reflex.
An adult human excretes, on an average, 1 to 1.5 litres of urine per day. The urine formed is a light yellow coloured watery fluid which is slightly acidic (pH-6.0) and has a characterestic odour. On an average, 25-30 gm of urea is excreted out per day. Various conditions can affect the characteristics of urine. Analysis of urine helps in clinical diagnosis of many metabolic discorders as well as malfunctioning of the kidney. For example, presence of glucose (Glycosuria) and ketone bodies (Ketonuria) in urine are indicative of diabetes mellitus.
DISORDERS OF THE EXCRETORY SYSTEM
Malfunctioning of kidneys can lead to accumulation of urea in blood, a condition called uremia, which is highly harmful and may lead to kidney failure. In such patients, urea can be removed by a process called hemodialysis. Blood drained from a convenient artery is pumped into a dialysing unit after adding an anticoagulant like heparin. The unit contains a coiled cellophane tube surrounded by a fluid (dialysing fluid) having the same composition as that of plasma except the nitrogenous wastes. The porous cellophane membrance of the tube allows the passage of molecules based on concentration gradient. As nitrogenous wastes are absent in the dialysing fluid, these substances freely move out, thereby clearing the blood. The cleared blood is pumped back to the body through a vein after adding anti-heparin to it. This method is a boon for thousands of uremic patients all over the world.Kidney transplantation is the ultimate method in the correction of acute renal failures (kidney failure). A functioning kidney is used in transplantation from a donor, preferably a close relative, to minimise its chances of rejection by the immune system of the host. Modern clinical procedures have increased the success rate of such a complicated technique.
Renal calculi: Stone or insoluble mass of crystallised salts (oxalates, etc.) formed within the kidney.
Glomerulonephritis: Inflammation of glomeruli of kidney.
SUMMARY
Many nitrogen containing substances, ions, CO2, water, etc., that accumulate in the body have to be eliminated. Nature of nitrogenous wastes formed and their excretion vary among animals, mainly depending on the habitat (availability of water). Ammonia, urea and uric acid are the major nitrogenous wastes excreted.
Protonephridia, nephridia, malpighian tubules, green glands and the kidneys are the common excretory organs in animals. They not only eliminate nitrogenous wastes but also help in the maintenance of ionic and acid-base balance of body fluids.
In humans, the excretory system consists of one pair of kidneys, a pair of ureters, a urinary bladder and a urethra. Each kidney has over a million tubular structures called nephrons. Nephron is the functional unit of kidney and has two portions – glomerulus and renal tubule. Glomerulus is a tuft of capillaries formed from afferent arterioles, fine branches of renal artery. The renal tubule starts with a double walled Bowman’s capsule and is further differentiated into a proximal convoluted tubule (PCT), Henle’s loop (HL) and distal convoluted tubule (DCT). The DCTs of many nephrons join to a common collecting duct many of which ultimately open into the renal pelvis through the medullary pyramids. The Bowman’s capsule encloses the glomerulus to form Malpighian or renal corpuscle.
Urine formation involves three main processes, i.e., filtration, reabsorption and secretion. Filtration is a non-selective process performed by the glomerulus using the glomerular capillary blood pressure. About 1200 ml of blood is filtered by the glomerulus per minute to form 125 ml of filtrate in the Bowman’s capsule per minute (GFR). JGA, a specialised portion of the nephrons, plays a significant role in the regulation of GFR. Nearly 99 per cent reabsorption of the filtrate takes place through different parts of the nephrons. PCT is the major site of reabsorption and selective secretion. HL primarily helps to maintain osmolar gradient (300 mOsmolL–1 -1200 mOsmolL–1) within the kidney interstitium. DCT and collecting duct allow extensive reabsorption of water and certain electrolytes, which help in osmoregulation: H+, K+ and NH3 could be secreted into the filtrate by the tubules to maintain the ionic balance and pH of body fluids.
A counter current mechanism operates between the two limbs of the loop of Henle and those of vasa recta (capillary parallel to Henle’s loop). The filtrate gets concentrated as it moves down the descending limb but is diluted by the ascending limb. Electrolytes and urea are retained in the interstitium by this arrangement. DCT and collecting duct concentrate the filtrate about four times, i.e., from 300 mOsmolL–1 to 1200 mOsmolL–1, an excellent mechanism of conservation of water. Urine is stored in the urinary bladder till a voluntary signal from CNS carries out its release through urethra, i.e., micturition. Skin, lungs and liver also assist in excretion.











No comments